This is the Weight and Healthcare newsletter! If you appreciate the content here, please consider supporting the newsletter by subscribing and/or sharing!
The public comment period has opened for the US Preventative Services Task Force’s massively ill-advised draft research plan “Weight Loss to Prevent Ob*sity*-Related Morbidity and Mortality in Adults: Interventions”
Here is the link to the plan text.
Here is the link to comment (you can also go to the link above and click “leave a comment” in the last line of the yellow box at the top of the page)
We have until June 14th to comment, please feel free to use anything I’ve written here for your comments.
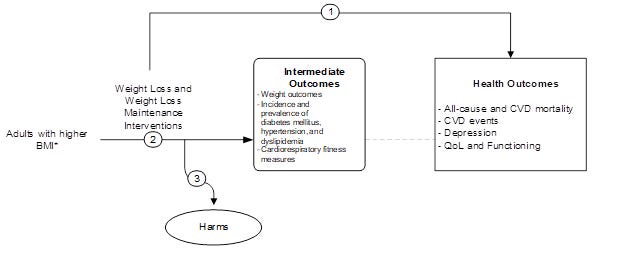
Their research can be summarized as: Observe weight loss interventions, observe outcomes, assume that all positive health outcomes are due to weight loss and not the behaviors changes that preceded both the (likely temporary) weight loss and the health changes, observe harms - kind of (butt we’ll get to that.) They’ve created a handy graph to explain:
Here are some ways that this goes wrong:
First, we have about a century of research showing that intentional weight loss attempts fail to create long-term, significant weight loss the vast majority of the time. Their inclusion criteria only requires studies to be 12 months long, when research shows that most weight is regained in years 2-5.
Next, we have research that tested the assumption that small amounts of weight loss cause improved health outcomes and did not find a causal link between the two (positing that behavior changes, social support, and access to healthcare may have been the reason for the health improvement.)
Supporting that, we have research showing that (understanding that health is not an obligation, barometer of worthiness or entirely within our control,) health-supporting behaviors are better predictors of current and future health that weight or weight loss attempts, and that intentional weight loss is not consistently associated with lower mortality.
But the USPSTF wants to do yet another study of short-term weight loss research that fails to discern between the impact of weight loss and the impact of behaviors. The fact that they are continuing to hammer this broken nail show that either they are simply misguided by their myopic belief in the weight=health, weight loss = health improvement paradigm/fantasy land, or this is being driven and/or supported by the weight loss industry.
If they move forward with this plan they will likely produce more “results” that uncritically claim that weight loss leads to health improvements without noting that the weight loss is not likely to last and that the health improvements could have been (and, in fact, likely were) acquired through health-supporting behaviors which, by themselves - extricated from attempts to manipulate body size, would have far less risk of harm.
But don’t take my word for it, let’s look at their “study aim” inclusion criteria:
Research they will include:
Weight loss or weight loss maintenance (they are including studies of “fair” or “good” quality, only excluding those deemed “poor”)
Research they will exclude:
Healthy lifestyle counseling with no weight-related messages
Primary prevention of weight gain
Treatment of cardiovascular disease
Management of diabetes
Treatment of cancer
They are literally excluding research that seeks to support health without weight loss. These are not the choices of researchers who want to find out the best way to support the health of higher weight people, these are the choices of researcher who want to continue to prop up a failed (but massively profitable) weight-loss paradigm.
They claim that they will be comparing weight loss interventions to “Weight-neutral healthy lifestyle intervention (i.e., diet and physical activity counseling with no weight loss message)” but without a clear plan to delineate to what extent any health improvements of weight loss interventions were actually due to behaviors, and without at least 5 years of follow-up to capture the high failure rate of weight loss interventions, this is essentially useless and, again, designed to prop up weight loss.
If they really want to do useful research they could:
Directly study the impact of health supporting behaviors on higher-weight people, excluding weight loss interventions.
Study the impacts of weight stigma, weight cycling, and healthcare inequalities on health outcomes for higher-weight people
At the very least, given the very well known long-term failure of intentional weight loss attempts (including weight loss drugs as soon as someone stops taking them) they should compare weight loss interventions to weight-neutral interventions utilizing long-term research of at least five years (and if the research doesn’t exist, then there is no reason for them to do this research, since we already have plenty of shoddy research of short-term weight loss interventions that fails to question whether any benefits are from the (likely temporary) weight loss or the behavior changes that preceded it.)
Still not convinced? Let’s take a look at their proposed “key questions”
Do primary care–relevant behavioral or pharmacotherapy weight loss and weight loss maintenance interventions for adults with higher body mass index (BMI) affect health outcomes?
Again, no mention here of controlling for the impact of health-supporting behaviors.
Do primary care–relevant behavioral or pharmacotherapy weight loss and weight loss maintenance interventions for adults with higher BMI affect weight outcomes or cardiometabolic outcomes?
Or, and hear me out, do health supporting behaviors impact cardiometabolic health outcomes?
What are the harms associated with weight loss interventions for adults?
There are so many issues with this:
People who conceptualize research like this are not likely to be qualified to identify harms.
A literature review is problematic because much of the research seems to go out of its way (accidentally or on purpose) to not capture adverse events
Almost none of the research that exists has appropriate follow-up to capture long-term harms
People who drop out of the interventions (sometimes over 60% of the study population) aren’t typically included in follow up (and typically are ignored by the study itself!) This means that those who dropped out due to harms and/or experienced harm later are highly unlikely to be captured.
Research that is undertaken to support the eradication of fatness has a strong tendency not to believe fat people when we talk about the harms of the interventions meant to eradicate us, and often works very hard to blame adverse events on the study subjects
Many weight loss interventions (and the people who support, conduct, and research them) are based on the belief that it’s worth risking higher-weight people’s lives and quality of life to make us thin, and thus harms are downplayed or considered reasonable “side-effects”
A large portion of weight loss research is funded and/or conduct by the weight loss industry with questionable/no attempts to capture harm
The “harms” they plan to include are:
Any adverse event or serious adverse event
Again, highly unlikely to be captured with any degree of accuracy and highly likely to capture far less than the actual incidence
Withdrawals or discontinuation of medication due to adverse effects
Some studies of weight loss medications include ONLY this as an adverse event, meaning that other adverse events fail to be captured
Unhealthy weight management efforts (e.g., using laxatives or self-induced vomiting) or eating patterns (excessive fasting, overly restrictive eating, or binging)
Note that a laxative effect and intervention-induced vomiting are side effects of some of the weight loss interventions they are including, but they don’t tend to count those as harms and, in some cases they consider them positive impacts since they can lead to (at least short-term) weight loss.
The use of “excessive” to modify fasting and “overly” to modify restrictive eating is a way to try to cover up the fact that they are literally prescribing these harms -symptoms of eating disorders (fasting and restriction) - to fat people. The concepts of “excessive” and “overly” are not scientific and do not have agreed upon definitions - also given the existence of weight loss interventions that prescribe as little as 800 or fewer calories per day, one wonders what their definition of “excessive” and “overly” might be?
Worsening of quality of life or psychological symptoms, including increased symptoms of depression and anxiety, and body image concerns
This is a loaded concept - Most weight loss studies show short-term improvement in these categories as people begin to (almost always temporarily) move themselves out of a stigmatized class and experience massive social approval. The studies almost always cease follow-up before the (almost certain) weight regain between 2-5 years and/or fail to follow-up with those who dropped out, thus failing to even attempt to capture long-term impact on these interventions.
Exercise-induced injury
I’m fine with this one, though it is rarely captured in studies so I have to wonder if it’s included here so that they can say it hardly ever happens?
I want to point out that they aren’t including the harms of weight cycling, which is the most common outcome of these weight loss interventions, or the harms of healthcare system interactions that are myopically focused on weight which can lead to missed diagnoses and patient disengagement as well as other harms.
I’ll say this one more time:
If they move forward with this plan they will likely produce more “results” that uncritically claim that weight loss leads to health improvements without noting that the weight loss is not likely to last and that the health improvements could have been (and, in fact, likely were) acquired through health-supporting behaviors which, by themselves - extricated from attempts to manipulate body size, would have far less risk of harm.
Here is the link to the plan text.
Here is the link to comment (you can also go to the link above and click “leave a comment” in the last line of the yellow box at the top of the page)
Again, the deadline for comment is June 14th, please feel free to use anything I’ve written here for your comments.
Did you find this post helpful? You can subscribe for free to get future posts delivered direct to your inbox, or choose a paid subscription to support the newsletter and get special benefits! Click the Subscribe button below for details:
Like the piece? Share the piece!
More research and resources:
https://haeshealthsheets.com/resources/
*Note on language: I use “fat” as a neutral descriptor as used by the fat activist community, I use “ob*se” and “overw*ight” to acknowledge that these are terms that were created to medicalize and pathologize fat bodies, with roots in racism and specifically anti-Blackness. Please read Sabrina Strings Fearing the Black Body – the Racial Origins of Fat Phobia and Da’Shaun Harrison Belly of the Beast: The Politics of Anti-Fatness as Anti-Blackness for more on this.



Submitted a full set of comments, backed up by the numerous resources you and others have amassed over the years. What a ridiculous load of B.S. this so-called research effort would have produced. Take that money and put it towards addressing community level wellness initiatives that make it safe for people to be outdoors, for example, or to have access to fresh produce.
Done! Tried my best to state concerns backed by research and just general research-flaws that they're making 👍🏻