This is the Weight and Healthcare newsletter! If you appreciate the content here, please consider supporting the newsletter by subscribing and/or sharing!
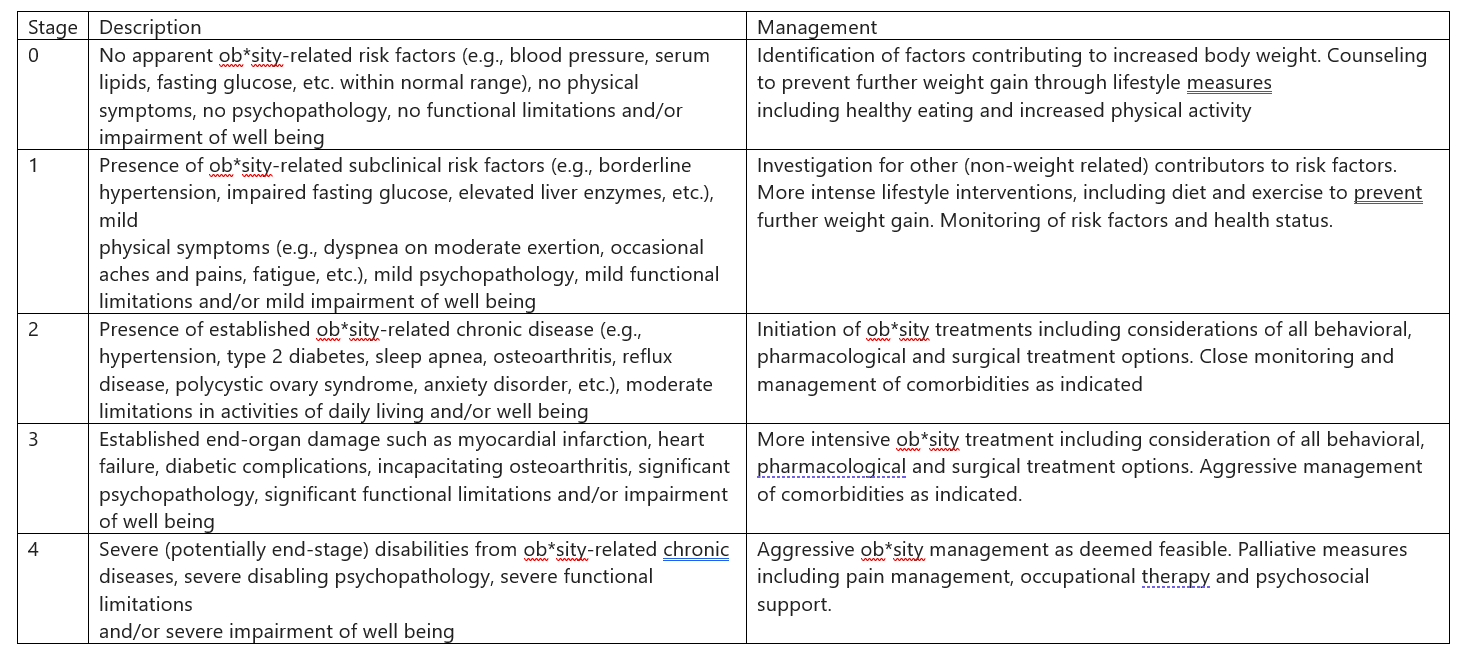
The Edmonton Ob*sity Staging System is, per its creators “a new simple clinical and functional staging system that allows clinicians to describe the morbidity and functional limitations associated with excess weight.” (A proposed clinical staging system for ob*sity, Sharma & Kushner, 2009)
Let’s take a look.
In their introduction, they admit that BMI and waist circumference measurements “do not provide information on presence or extent of comorbidities or functional limitations that would guide decision making in individuals.” That is accurate. However, instead of taking the logical next step and acknowledging, or at least considering, that there is no need to classify people by weight, they instead go looking for a new and different way to classify fat* people.
That they would do this is not surprising. Now, they are likely not coming from a place of wanting to intentionally harm higher-weight people. In fact, I was once on a news program with Dr. Sharma and some personal trainer from some reality show (I can’t remember his name or the show,) whose plan to combat my knowledge and lived experience was interrupting and insulting me. Dr. Sharma was kind and protective. He seems to come from the “Don’t stigmatize fat people, but do risk their lives and quality of life to make them thin camp.)
Arya Sharma was, at the time of publication of this study, Chair for Ob*sity Research and Management, University of Alberta. He is now the founder and director of the Canadian Ob*sity Network (a group much like the Ob*sity Action Coalition that claims to advocate for higher-weight people but, in fact, is predominantly funded by, and acts as a lobbying arm for, the weight loss industry.) Their original name was The Canadian Ob*sity Network, which gave them my favorite acronym for one of these orgs until they changed their name to Ob*sity Canada. Their current “corporate supporters” include Novo Nordisk, Boehringer Ingelheim, Nestle Optifast, TOPS Club, and Weight Watchers. He is also the past-president of the Canadian Association of Bariatric Physicians and Surgeons and has received speaker’s bureau and consulting fees from Novo Nordisk. (Canada’s laws about payment disclosure are more lax than those in the US, so Canadian doctors can take untold amounts of money with no disclosure as to amounts.)
Robert Kushner bills himself as a “world renowned weight management expert” and “the author (or editor) of 12 books, 58 book chapters and nearly 200 scientific articles on overweight, ob*sity and nutrition, Dr. Kushner has a unique skillset to help you reach your weight loss goals.” (I do want to point out that not one of those 200 articles offers any proof that his methods lead to significant, long-term weight loss for more than a tiny fraction of people.) Per openpayment.cms.gov he has taken $429,988.30 in general payments and another $327,375.70 in research and associated research funding between 2015 and 2021, predominantly from Novo Nordisk.
So, while they may not be trying to intentionally harm fat people, they have both absolutely pinned their careers on so-called “ob*sity medicine” (aka: body-size-as-disease/weight-loss-as-cure model) which may be why they didn’t investigate if, as research suggests (with the understanding that weight and health are not barometers of worthiness and are far from being entirely within our control) supporting the health of fat people rather than trying to manipulate their body size would create greater benefits with fewer risks.
Instead, they created a staging system, claiming:
The rationale for a clinical staging system is also based on the notion that patients with current health problems related to ob*sity should be treated more aggressively and that in the context of limited resources, a staging system must aid in the equitable identification and prioritization of patients, who would most likely benefit from aggressive and resource-intensive weight management.
The problem with this is that health issues that are considered “related to ob*sity” are health issues that happen to people of all sizes. The research that is used to show the correlation (without causation) between weight and these healthcare issues is often funded by the weight loss industry and/or conducted by its employees or researchers to whom they make payments. This research rarely mentions, let alone controls for, the impact of well-known confounding variables including weight stigma, healthcare inequalities, and weight cycling, which is, by far, the most likely outcome of weight loss attempts. All three of these are also driven by the idea of pathologizing higher-weight bodies that is inherent in the EOSS.
They also don’t identify any study that shows that “aggressive and resource-intensive weight management” that they recommend creates significant long-term weight loss or improved health, which are two separate things.
In trying to justify this, they bring up things like staging systems for kidney disease and cancer. They don’t point out that these are completely different than the EOSS since these are staging systems for people with shared symptomology, not simply shared size. There isn’t, for example, a separate staging system for people with these symptoms who are also tall, or who are also brunette, even though, technically, you could create such a system as they have done with the EOSS and healthcare issues that happen to people of all sizes.
With that, let’s look at their so-called “stages” of “ob*sity”:
Now let’s consider what we would have to buy into in order to believe that this is a good idea.
Note that even at stage zero they are still recommending weight loss industry interventions with no proof of efficacy, so they are still pathologizing bodies based on a height-weight ratio and regardless of their actual health/symptomology/cardiometabolic profile.
Every single symptom and situation on the “description” list is something that also happens to thin people. So, we are to believe that when these things happen to fat people, they are due to their fat, but when they happen to thin people they are due to…something else.
Next, we are to believe that weight loss is the solution, despite the fact that these things all happen to thin people who are offered treatment options that are massively more successful than behavior-based weight loss interventions (which fail about 95% of the time and have the opposite of the intended effect up to 66% of the time) and far less dangerous than diet drugs or weight loss surgeries (which, remember, take a healthy digestive system and surgically create a disease state.)
Also, note the intersection of weight stigma and ableism – if you are fat, disabled, and have other health issues then (these authors believe) it’s reasonable to risk your life and quality of life to make you thin despite, again, the existence of disabled thin people with those same health issues (who, to be clear, can also face a massive amount of ableism.)
Further, when looking at things like “functional limitations” or “impairment of well being” what they may actually be measuring is experience of weight stigma, including structural weight stigma in which the things and places that fat people want to use and access are created for thin bodies/to the exclusion of fat bodies. This places the impetus on the victims of stigma to change, rather than focusing on increasing access and accommodation.
Similarly, when looking at psychopathology, there is no discussion of the ways in which living in a world rife with weight stigma can impact mental health, instead choosing to suggest that those whose oppression impacts their mental health should change themselves to suit their oppressors (risking their lives and quality of life in the process.)
Regardless of what one believes about weight and health, the idea that the victims of oppression should have to change themselves to suit their oppressors/escape the oppression is always wrong.
In part 2 we’ll take a look at a study that Dr. Sharma and other authors created to test the validity of this system.
Did you find this post helpful? You can subscribe for free to get future posts delivered direct to your inbox, or choose a paid subscription to support the newsletter and get special benefits! Click the Subscribe button below for details:
Like the piece? Share the piece!
More research and resources:
https://haeshealthsheets.com/resources/
*Note on language: I use “fat” as a neutral descriptor as used by the fat activist community, I use “ob*se” and “overw*ight” to acknowledge that these are terms that were created to medicalize and pathologize fat bodies, with roots in racism and specifically anti-Blackness. Please read Sabrina Strings Fearing the Black Body – the Racial Origins of Fat Phobia and Da’Shaun Harrison Belly of the Beast: The Politics of Anti-Fatness as Anti-Blackness for more on this.
Note I don’t link to everything I discuss in this post because I don’t want to give traffic and clicks to dangerous media.




I had borderline high bp as a 12 year old. I had a normal BMI at the time, but my borderline high bp persisted and when I began trying to conceive, my doctor put me on blood pressure medication for the first time. I have stayed on the same dose throughout my pregnancies, it's now been 7 years since I was put on this dose. And yet when I went to a new doctor, he tried to suggest my BP was related to my current weight. The healthcare industry is ridiculously fatphobic and led to believe issues are caused by being fat. My grandmother who has always benefited from thin privilege has also been on blood pressure meds for 65 years, and I suggested this as a strong genetic component to the dr. He looked at me skeptically. I am a small fat person, and I usually don't have problems seeking medical care or hearing weight loss comments so I thrown for a loop last week with this encounter. the staging system seems unhelpful at best, and damaging at worst. How does this benefit any fat person?
Thank you, as always, Ragen, for a thorough piece on this issue.