This is the Weight and Healthcare newsletter! If you like what you are reading, please consider subscribing and/or sharing!
A reader asked if all of the options for weight loss (bariatric) surgery were equally risky. Before we dig into it, I first want to note that this piece will talk frankly about the physical and psychological harm of these procedures.
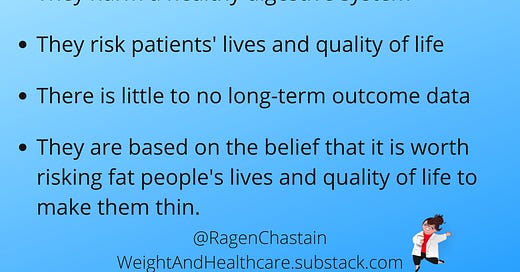
What these surgeries have in common is that they take a perfectly healthy digestive system and purposefully create a disease state (forced restriction and/or malabsorption) that risks the life and quality of life of the patient with no guarantee of long-term weight loss or health improvement (which are two separate things.) There is very little long-term outcome data beyond about 10 years, meaning a proper informed consent conversation is basically impossible, and these procedures are essentially experimental.
We do know that, while these surgeries are often enthusiastically marketed to consumers using the stories of those who are happy (often in the “honeymoon” phase of the first 1-3 years post-procedure,) many survivors of these procedures experience life-long horrific side effects and would give anything to take the surgeries back (they are typically not asked to participate in marketing efforts.) Others have died and don’t have the opportunity to tell their stories (again, you won’t find videos about their stories on the websites of the healthcare facilities that aggressively sell these procedures.) Adding to the issue, those involved in the industry that profits from these surgeries often work very hard to blame patients for negative outcomes.
It's also important to understand that the belief that underpins these procedures is that it’s worth risking fat people’s lives and quality of life to make them thinner (and/or to “treat” health issues that thin people also get and for which they are not asked, let alone recommended, to take these risks.) I do not personally believe that these surgeries meet the basic requirements for ethical, evidence-based medicine, but I also take a firm view on body autonomy and so my goal is not to shame people who have chosen these procedures when they were offered, only to offer information.
Let’s look a the different options. As always, in situations where studies come from a place of weight stigma I don’t link to them, but provide enough information for them to be found.
Gastric Balloon (Orbera)
This balloon is placed in the stomach and then filled with saline. It “works” by taking up space to create food restriction. (There are other similar options, including plenity, that work on the same idea – basically, fill the stomach with something that is not food in order to disrupt the body’s hunger signals.)
In the initial study, the average participant lost 21.8 pounds in 6 months then gained back 5.6 pounds in the following 6 months, at which point they stopped tracking (in the hopes, I imagine, that people would assume that the weight regain stopped the day they stopped tracking it.)
Haddad et al. in 2019 found that after three years “The vast majority of patients (78.7%) regained weight.” It is important to note that studies of other intentional weight loss options show that people regain all of their weight within five years, so that 78.7% may well continue to climb.
So what did patients risk for a little (very likely temporary) weight loss? Orbera’s own study showed that 160 subjects had a total of 810 “device-related adverse events” over 6 months.
Death is possible, due to complications related to gastric or esophageal perforation, and intestinal obstruction.
Within months of launch, five people died within a month of having the procedure, three died within just three days. The FDA also received reports of two additional deaths — one from gastric perforation, the other from esophageal perforation.
Gastric Banding (Lap Band)
This procedure binds the stomach to make it smaller and force food restriction. It has a high rate of people regaining to, or close to, baseline and a high rate of complication and re-operation rates (with some studies finding it as high as 60%.)
Ibrahim et al. looked at Medicare patients who got the procedure between 2006 and 2013 and found that by 2013, 77.3% of the money that Medicare was spending on gastric banding was for re-operations.
Common side effects include difficulty swallowing and severe nausea and vomiting (including multiple times a day,) esophageal dysmotility, esophageal dilation or esophagitis, band slippage (which may require emergency surgery,) and band erosion (that typically causes long-term port infections.)
These surgeries often end in weight gain, at which point more drastic (and risky) weight loss surgeries are frequently recommended. They are marketed as reversible, but reversal can be complicated and can leave people with lifelong physical and psychological harm.
Gastric Sleeve
This surgery removes 80-85% of the stomach, and staples the rest together. It “works” by forcing food restriction.
Side effects include (but are definitely not limited to) gastrointestinal obstruction, hernias, gastroesophageal reflux, hypoglycemia, malnutrition, and vomiting, and the surgery and side effects can be fatal.
Many patients regain weight after the first 1-3 years, with some studies showing that a quarter of surgery survivors have regained back to their baseline within 10 years (There is very little data after ten years.)
The surgery is not reversible, and regardless of side effects and/or failure to lose weight or experience of weight regain, patients will never regain the functionality of the digestive system that they had before the surgeries.
Roux-en-Y, Gastric Bypass
This surgery reduces the stomach to roughly the size of a walnut and attaches it to the small intestine (bypassing the duodenum and part of the jejunum - about 30% of the small intestine). It “works” by forcing food restriction and purposefully creating a malabsorptive state (forcing the body to fail to properly digest food.)
Side effects are numerous, can have severe impact on quality of life, and the surgery can result in death. There is a full list here.
Weight regain is common with this surgery as well, with a study showing that only 40% maintained at least a 30 percent weight loss after 12 years.
Survivors of the surgery will never again be able to get all of their nutrition from food and must maintain access to expensive supplements for the rest of their lives or face serious, possibly life-threatening consequences.
While these surgeries are sometimes sold as reversible, patients are extremely unlikely to regain the fully functioning digestive system they had prior to the surgery.
Duodenal Switch
This surgery combines Sleeve Gastrectomy with an intestinal bypass, but where Rouy-n-Y bypasses about 30% of the intestine, this surgery bypasses about 75% of the intestine forcing food restriction and creating severe malabsorption.
This surgery is even more dangerous than gastric bypass, and for that “reason” is recommended for people at higher BMIs which is a clear example of weight stigma in healthcare, since predicating risk on body size suggests that people’s lives and quality of life are less valuable at higher weights.
Bariatric Revision
This is a surgery that is performed on survivors of gastric bypass or sleeve who aren’t happy with the amount of weight loss and/or have regained weight. It further reduces the pouch (formerly known as the stomach) to the size of a dime, forcing further restriction and creating additional risk of side effects.
To learn more about weight loss surgery, you can check out my previous three-part series:
The Basics
Weight Loss Surgery and Type 2 Diabetes
Weight Loss Surgery - Long-Term Outcomes and Informed Consent
Did you find this post helpful? You can subscribe for free to get future posts delivered direct to your inbox, or choose a paid subscription to support the newsletter (and the work that goes into it!) and get special benefits! Click the Subscribe button below for details:
More research and resources:
https://haeshealthsheets.com/resources/
*Note on language: I use “fat” as a neutral descriptor as used by the fat activist community, I use “ob*se” and “overw*ight” to acknowledge that these are terms that were created to medicalize and pathologize fat bodies, with roots in racism and specifically anti-Blackness. Please read Sabrina Strings’ Fearing the Black Body – the Racial Origins of Fat Phobia and Da’Shaun Harrison’s Belly of the Beast: The Politics of Anti-Fatness as Anti-Blackness for more on this.



And all of these barbaric procedures are based on the notion that fat people are fat because we eat more than non-fat people. Which is blatantly untrue. My husband regularly marvels at how little I actually eat yet here I am, still fat.
They can all eff off.
I'm stunned! This is horrific, how can they get away with this? My niece is currently waiting for surgery (I don't know which one) she's so incredibly fat phobic that she will do anything "to be thin". They're selling it to her by using her young daughter - gaslighting her saying things like, setting a good example, being there for her when she grows up (implying she's going to die). I really don't know what to say to her. I've tried to introduce her to fat positivity but nothing works. I post a lot about fat positivity, I'm currently on a medication for my disability, one of the side effects is weight gain and it's been fantastic! Yes I've gained weight, but my mobility is so much better & I can now walk with sticks! It really is awesome. But all she sees is the weight not the improvement in my life.