This is the Weight and Healthcare newsletter! If you like what you are reading, please consider subscribing and/or sharing!
In part 1 we examined the massively misleading opening claim of the abstract of the new study “Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial” by Ryan et al, published in the journal naturemedicine, and we looked at the magnitude of the conflicts of the authors. Today I’ll dig into the rest of the study.
Before I do, I want to send some quick gratitude to my paid subscribers. To be clear, whether you’re a paid subscriber, free subscriber, or just found this piece randomly, I am deeply grateful that you are here. That said, pieces like this have a quick turnaround (so that the people who need the information have it available, since the Novo Nordisk marketing machine is already in full swing,) and they require many hours of work. Paid subscriptions make that possible for me to do, so thank you!
Let’s get into this:
Their “Main” section begins with some problematic claims (shown in italics):
“The World Health Organization defines clinical obesity as ‘abnormal or excessive fat accumulation that may impair health.”
That’s not a scientific definition of “clinical” anything. First of all, “may impair health?” How are we determining that? How are we defining “abnormal” or “excessive” how are we defining “impair” and how are we differentiating health “impairments” that are supposedly “caused” by whatever “abnormal or excessive fat accumulation” is, from the exact same “impairments” that happen to thin people? I wrote about this in-depth here but we have to start demanding more of science than a “clinical definition” that was driven by the weight loss industry to give them the largest possible market.
“Excess abnormal body fat, especially visceral adiposity and ectopic fat, is a driver of cardiovascular (CV) disease (CVD)3,4,5, and contributes to the global chronic disease burden of diabetes, chronic kidney disease, cancer and other chronic conditions”
Again, no definition for “excess abnormal body fat” and visceral and ectopic fat exists at varying levels in people of all sizes. They cite three references for this:
1. An article by a group called “the “Global Burden of Disease (GBD) 2015 Ob*sity Collaborators” looking at data between 1980 and 2015 that was based on estimates they created including of the rates of “ob*sity and ov*rweight,” the supposed “disease burden attributable to high body mass index (BMI)” and “high BMI-attributable deaths… and other measures” (Global Burden of Disease Study 2015 (GBD 2015) Obesity and Overweight Prevalence 1980-2015)
2. 2013 guidelines co-written by the weight loss industry group The Ob*sity Society (2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society)
3. A 2005 article written by authors including members of the Weight Watchers advisory board, all but one of whom had conflicts of interest in the weight loss industry (Ob*sity and Cardiovascular Disease: Pathophysiology, Evaluation, and Effect of Weight Loss)
So let’s review – it is 2024, and they are making sweeping claims about the impact of weight on health that underpin their entire argument that these medications are worth the (significant) risks and costs…and this is what they’ve arrived at to support their claims? Really?
The three references they chose take a simple correlation/causation approach that should be shouted down in any legitimate statistics or research methods class, namely assuming that if health issues happen to higher-weight people, it’s because of their weight. They each fail to control for (or even mention) the confounding variables of weight stigma, weight cycling, and healthcare inequalities. So, the “science” here shakes out that if a higher-weight person has type 2 diabetes, it’s because they are higher-weight and it gets credited to the “global disease burden” of higher-weight people. If a lower-weight person has type 2 diabetes it’s due to…something else. Sure, that checks out (/sarcasm.)
We also get:
“Remediating the adverse health effects of excess abnormal body fat through weight loss is a priority in addressing the global chronic disease burden.”
And here we have the second part of this fallacy – it starts with “if higher-weight people have health issues, then their weight is the cause” and ends with “and weight loss will solve it.” Again, this is despite the fact that these health issues happen to thin people, and that there are significant confounding variables here (This also isn’t remotely new information. Over twenty years ago Bacon and Aphramor found that the entirety of excess mortality that was associated with “ob*sity” in Framingham and the NHANES could actually be due to the negative impacts of weight cycling and there is no excuse for not including this in their analysis. There is a list of research around this here.)
They base this on the uncritical assumption that if people make behavior changes and experience both health benefits and weight loss, then the weight loss is what created the health changes. This ignores both the behavior changes in the subjects as well as research showing that behavior changes lead to health changes without weight changes. (I’ll get more deeply into this in a moment.)
Finally, let’s examine this claim:
“Data derived from the SELECT trial offer the opportunity to evaluate the weight loss efficacy, in a geographically and racially diverse population”
In terms of geographical diversity, they had study sites in Argentina, Australia, Austria, Belgium, Bulgaria, Brazil, Canada, Colombia, Czech Republic, Germany, Denmark, Algeria, Spain, Finland, France, United Kingdom, Greece, Croatia, Hungary, India, Ireland, Israel, Italy, Japan, Latvia, Mexico, Malaysia, Netherlands, Norway, Poland, Portugal, Romania, Russian Federation, Serbia, Thailand, Turkey, Taiwan, Ukraine, United States of America and South Africa.
Yet it seems that their threshold for “racially diverse” is pretty low given that even with all of those sites, 83.9% of subjects in the semaglutide group and 84.1% of subjects in the placebo group were white.
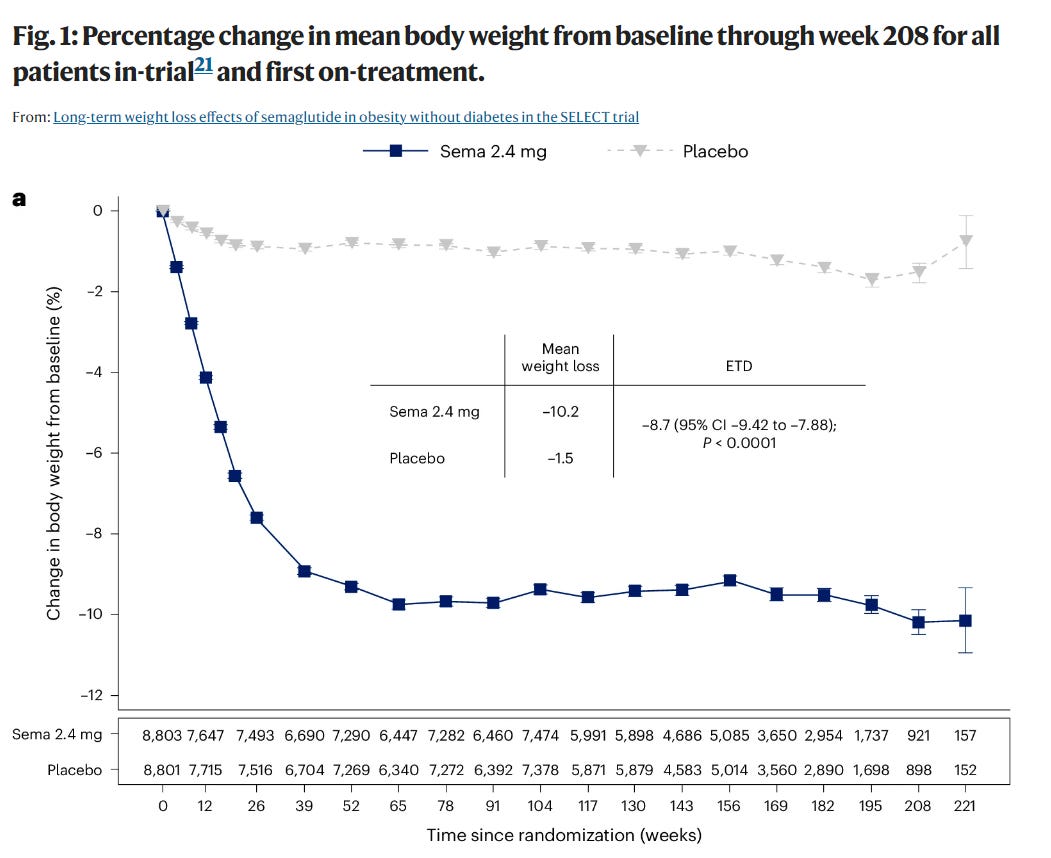
Now let’s dispense with the main claim being made (and the one that I’m seeing most commonly repeated in the press) “In patients treated with semaglutide, weight loss continued over 65 weeks and was sustained for up to 4 years. At 208 weeks, semaglutide was associated with mean reduction in weight (−10.2%), waist circumference (−7.7 cm) and waist-to-height ratio (−6.9%) versus placebo (−1.5%, −1.3 cm and −1.0%, respectively; P < 0.0001 for all comparisons versus placebo).”
First, note that weight loss leveled off at 65 weeks. The idea being that whatever someone has lost at 65 weeks is pretty much it and, best case scenario, they can keep it off by taking this medication for the rest of their life.
The words “up to” (as in “sustained up to 4 years”) are doing a lot of work here. For example, if I said that I have been in up to 10 Broadway shows, I could mean that I’ve been in 9 Broadway shows. But I could also mean (accurately) that I’ve been in 0 Broadway shows (at least for now, call me!)
The quick story here is told by Figure 1:
Now, the line sure does look like subjects were maintaining an average 10% loss of body weight. But look with me at the little numbers underneath. Those are the participants at each time interval. You’ll note that the treatment group starts with 8,803. At 104 weeks (2 years) they have 7,474 people left and average weight ticks up. Then we see an overall decline to just 921 subjects in the treatment group at 208 weeks and by 221 weeks they were down to just 157 in the treatment group and 152 in the placebo group.
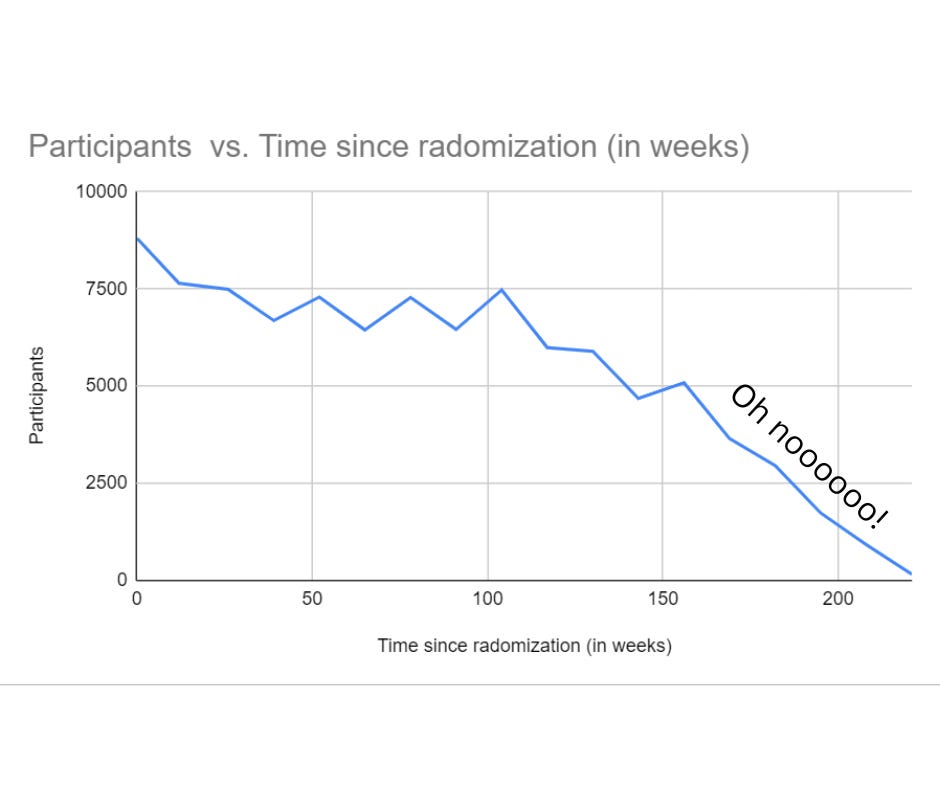
I made my own chart to create a visual representation of the treatment-group participant attrition
Given this information, alternate names for this study might be:
Only the people who aren’t regaining weight come back for the weigh-ins
Only the people who are able to crash diet enough to make their weight look stable come back for the weigh-ins
Most people don’t make it 4 years on Semaglutide 2.4mg, which must be taken for life to even maybe perhaps have a chance, however small, of maintaining a small amount of weight loss
Let’s look at the next claim:
“Clinically meaningful weight loss occurred in both sexes and all races, body sizes and regions.”
Again, the population is massively skewed toward cis men and white people. Also, their definition of “clinically meaningful” is based on a myth that was created chiefly by the weight loss industry and did not hold up to the scrutiny of actual research– namely that 5-10% weight loss “creates clinically meaningful health benefits.” This myth is built on making no attempt to separate the impact of behavior changes (that precede both the health changes and the small, likely temporary weight changes) from the impact of weight loss and, instead, crediting any health improvements to small amounts of simultaneous weight loss. Nice work if you can get it. I wrote about this myth in detail here.
At this point you may be screaming “Enough with the averages already. Just tell us how much weight they lost already!” (or maybe that’s just me.) Regardless, this is as close as they get:
“Among in-trial (intention-to-treat principle) patients at week 104:
67.8% lost ≥5%, 44.2% lost ≥10%, 22.9% ≥15%, 11% lost ≥20%, and 4.9% lost ≥25%”
Let’s say this another way:
32.2% failed to lose even 5% of body weight, 55.8% failed to lose 10%, 77.1% failed to lose 15% or more, 89% failed to lose 20% or more, and 95.1% failed to lose 25% or more (and remember that weight loss leveled off at about 65 weeks.)
They also make claims about the percentage of patients who moved from one BMI category to another (stacking the deck by using the extremely questionable “classes” of “ob*sity” to create as many categories as possible.) Given the small amounts of weight loss, this seems to only acknowledge how many people were simply on a BMI cusp to begin with (and also the problematic nature of BMI and other composite measures .)
I also have some other questions here.
First, why are they reporting information for 104 weeks when they have data for 208 weeks? If it’s because there were so few participants left at 208 weeks, then why would they make any claims at all about their four-year outcomes?
Also, why are they using the SELECT trial population which focused on cardiovascular disease (and which heavily skewed toward both cis-male and white, average age 61.6, all participants had to have existing cardiovascular disease and not have Type 2 Diabetes,) to claim long-term weight loss rather than talking about the STEP trial population (which while heavily skewed toward cis-woman and even more skewed white) had an average age of 47.3 and, oh yeah – was actually about weight loss (and which I wrote about in detail here)?
They talk about this a bit, but make the (odd, to me, at least) choice to compare the 104-week SELECT (cardiovascular) trial to the 68-week STEP 1 (weight loss) trial, rather than the 104-week STEP 5 (weight loss) Trial.
STEP 1 shows that those in the treatment group (with all the limitations we’ve talked about) lost an average of 4.5% more than those in the SELECT trial compared to their respective placebo groups. The authors suggest that this might be because SELECT was designed as a cardiovascular outcomes trial and not a weight-loss trial so those in STEP 1 were desirous of weight loss as a reason for study participation and/or because they received structured lifestyle intervention (which included a −500 kcal per day diet with 150 min per week of physical activity).
That may be true, but we also know that about 100 years of research show that structured lifestyle interventions lead to short-term weight loss but almost always long-term weight regain and so I am much more interested in 4-year outcomes in the STEP Trial participants and remain curious as to why they are choosing to follow and publicize this (cardiovascular trial) population instead?
So let’s look at their overarching claims. In their discussion section, they really go for the gold:
“These data, representing the longest clinical trial of the effects of semaglutide versus placebo on weight, establish the safety and durability of semaglutide effects on weight loss and maintenance in a geographically and racially diverse population of adult men and women with overweight and obesity but not diabetes. The implications of weight loss of this degree in such a diverse population suggest that it may be possible to impact the public health burden of the multiple morbidities associated with obesity. Although our trial focused on CV events, many chronic diseases would benefit from effective weight management.”
This seems to me to be much more like marketing language than anything resembling a scientific discussion. First of all, again, why are they using the trial in which weight was a secondary endpoint, rather than the trial where it was the primary endpoint? Why are they making broad safety and efficacy claims for a time frame during which the trial lost 89.5% (7,882 of the original 8,803) of the treatment group participants? They “support” their claim that “many chronic diseases would benefit from effective weight management” with a single citation which is a speculative editorial (Treating chronic diseases without tackling excess adiposity promotes multimorbidity) whose authors take a ton of money from the weight loss industry, including Novo Nordisk.
Note that this trial, like all of Novo Nordisk’s trials, failed to include a weight-neutral comparator group to see if any health benefits could be achieved through weight-neutral, health-supporting behaviors without the risks and expense of this medication. Also, though Semaglutide by injection is available in therapeutic doses starting at .5mg, they only tested the 2.4mg weight loss dose here (with people taking less only when they couldn’t tolerate the target dose.) I wonder if it’s because that’s the dose for which they are pushing for Medicare and insurance coverage right now.
One more time, again using the language “racially diverse population of adult men and women with overweight and obesity” is ludicrous for a study population that is over 80% white and 72.3% cis male with a lowest possible age of 45 and an average age of 61.6.
They also claim:
“Furthermore, the weight loss was sustained over 4 years during the trial.”
Not to belabor this, but (besides all the issues we’ve already covered,) they seem to be comfortable with this claim even though they lost almost 90% of the participants in the treatment group.
Let me just say this: if a 6th grader was studying whether fruit flies live longer eating bananas or apples for the science fair, and somehow 89.5% of the fruit flies escaped between the halfway point and the end point of the study, and that kid concluded with total confidence that “this project establishes the safety and durability of bananas on increasing the lifespan of fruit flies” and drew a graph and called it a day, that kid would…well, let’s just say they would not be in contention to win the 6th grade science fair but they would be in contention for a conversation with their 6th grade teacher to help them with some of the very important basic science concepts that they had obviously missed.
Let’s please hold medical research (including and especially research where the researchers have taken millions from the company whose product is being researched and/or where the research is funded and/or conducted by people with a financial interest in the results,) to a higher standard than we hold elementary school science fair projects.
Did you find this post helpful? You can subscribe for free to get future posts delivered direct to your inbox, or choose a paid subscription to support the newsletter (and the work that goes into it!) and get special benefits! Click the Subscribe button below for details:
Liked the piece? Share the piece!
More research and resources:
https://haeshealthsheets.com/resources/




Great analysis- thanks. As a recovering data scientist with a particular interest in data visualization, your "Participants vs Time" graph made me laugh out loud, Way to make a point!
You have an amazing ability to translate all the research babble into clearly understandable language for us mortals — thank you!! It still baffles and angers me that diet culture can get away with this nonsense.